- Solutions Solutions
Explore how Aidoc’s clinical AI solutions can increase hospital efficiency, show proven return on investment, and help enable better outcomes.
Learn moreImproving the lives of patients across the care continuum
Setting the standard for neuro care with real time notification
Automatically analyze imaging to rapidly identify abnormalities
- Platform Platform
Discover how Aidoc’s AI platform offers seamless end-to-end integration into a facility’s existing IT infrastructure enabling implementation of AI at scale.
Learn moreaiOSTMAidoc’s proprietary enterprise platform to reliably deploy, measure and run AI at scale
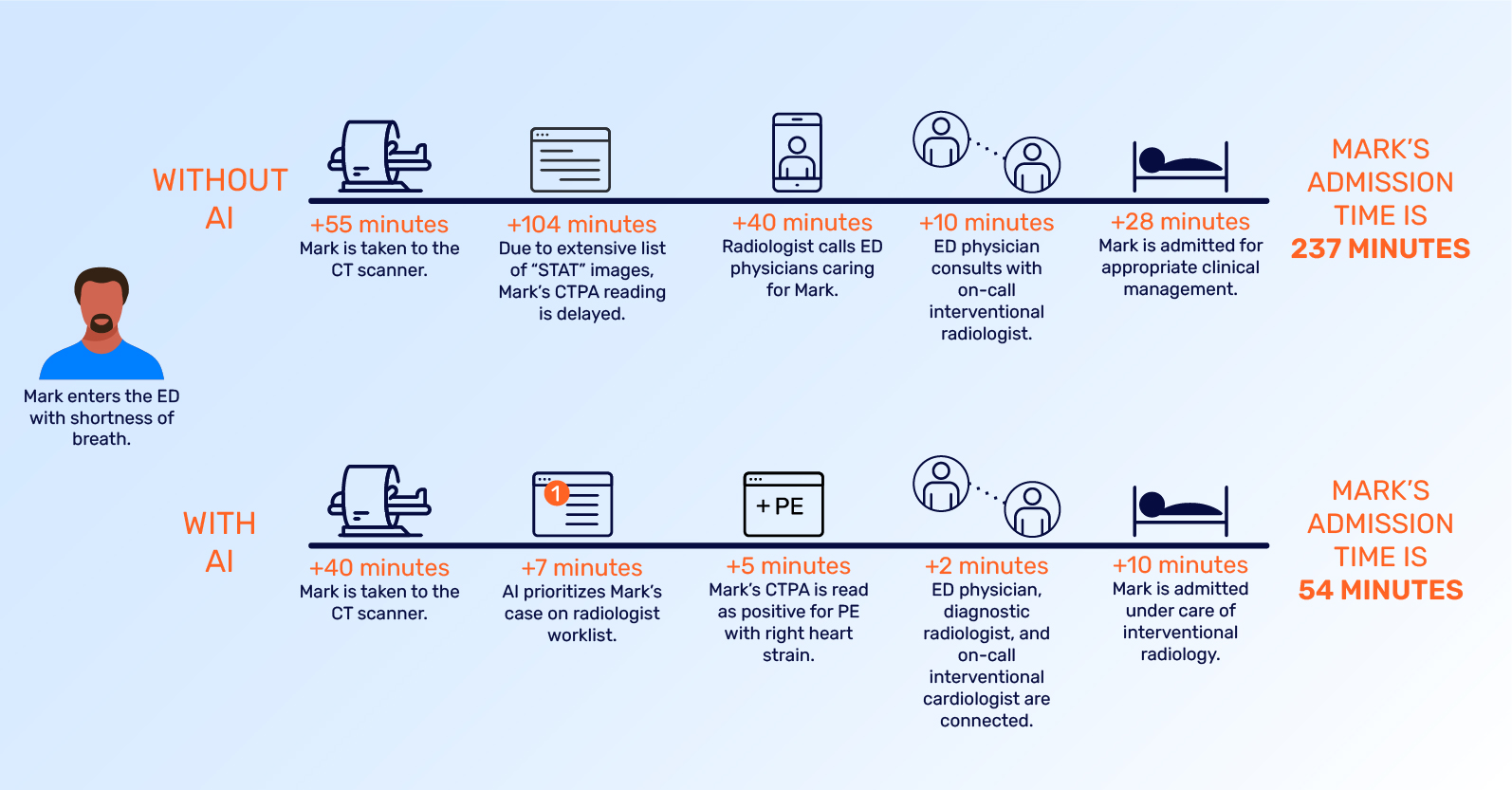
Care CoordinationAlerts the right users across the imaging and clinical workflow expediting decision-making
Systems IntegrationsCustom configured and integrated into existing systems with minimal effort from IT teams
PartnersVetted third-party algorithm developers and OEMs for the industry’s most complete platform
- Healthcare AI Healthcare AI
Information and resources about AI transformation rooted in real-world experiences.
Learn MoreLearn how to go beyond the algorithm to develop a scalable AI strategy and implementation plan.

- Learn Learn
See the latest research, case studies, tips and more to start improving outcomes with healthcare AI today.
Learn moreResources - Learn Learn
See the latest research, case studies, tips and more to start improving outcomes with healthcare AI today.
Learn more - Company Company
Learn more about Aidoc’s approach, mission and leadership team that is revolutionizing healthcare with AI.
Learn more - Book a Meeting
- Search
- Solutions Solutions
Explore how Aidoc’s clinical AI solutions can increase hospital efficiency, show proven return on investment, and help enable better outcomes.
Learn moreImproving the lives of patients across the care continuum
Setting the standard for neuro care with real time notification
Automatically analyze imaging to rapidly identify abnormalities
- Platform Platform
Discover how Aidoc’s AI platform offers seamless end-to-end integration into a facility’s existing IT infrastructure enabling implementation of AI at scale.
Learn moreaiOSTMAidoc’s proprietary enterprise platform to reliably deploy, measure and run AI at scale
Care CoordinationAlerts the right users across the imaging and clinical workflow expediting decision-making
Systems IntegrationsCustom configured and integrated into existing systems with minimal effort from IT teams
PartnersVetted third-party algorithm developers and OEMs for the industry’s most complete platform
- Healthcare AI Healthcare AI
Information and resources about AI transformation rooted in real-world experiences.
Learn MoreLearn how to go beyond the algorithm to develop a scalable AI strategy and implementation plan.

- Learn Learn
See the latest research, case studies, tips and more to start improving outcomes with healthcare AI today.
Learn moreResources - Learn Learn
See the latest research, case studies, tips and more to start improving outcomes with healthcare AI today.
Learn more - Company Company
Learn more about Aidoc’s approach, mission and leadership team that is revolutionizing healthcare with AI.
Learn more - Book a Meeting
- Search