I was reading a Politico article the other day titled “Artificial intelligence was supposed to transform health care. It hasn’t.” The headline was certainly thought provoking. It also shined a light on the fact that there are lingering misconceptions surrounding the effectiveness of Artificial Intelligence (AI) in healthcare. The truth is that the impact of healthcare AI has already arrived, and despite the groundbreaking transformations we’ve already seen, I anticipate that its impact will multiply tenfold in the next five years as it becomes more deeply developed and widely adopted.
AI has been commercially available in healthcare settings since 2019. In just three years, the impact of healthcare AI has proven to be massive, as I will touch on in this article. With that said, I feel an even greater sense of excitement for what’s yet to come.
I do believe that the expectations surrounding healthcare AI need to be adjusted. AI should not be looked at as a ‘savior’ for healthcare, but as a tool that empowers physicians with “superhuman” capabilities. I see AI as one of the few burgeoning technologies that will help health systems rise above some of today’s challenges and operate at an even higher standard.
AI Today: Augmentation, Not Replacement
AI cannot replace a physician. Coming from someone with a deeply vested interest in the success of healthcare AI, this may come off as counterintuitive. But the truth remains: AI is not meant to replace physicians, but to augment them.
As the Politico piece notes, there have been dystopian-esque perspectives like that of Geoff Hinton in 2016, proclaiming that AI would phase out radiologists within five years. While AI does have the power to drive automation in healthcare, not all industries where AI can be applied are equal in that sense. Manufacturing or banking industries are not like healthcare.
Despite sparsely published studies showing AI outperforming radiologists under specific conditions, the reality of real-world integration of AI into healthcare demonstrates time and again the complementary and synergistic role between physicians and AI. For example, Envision Healthcare, in studying the impact of AI on identifying lung blood clots, observed that while AI might have been more effective at identifying true positive cases, the radiologist was stronger at identifying true negatives. They concluded:
“When the exceptional AI sensitivity is coupled with the superior radiologist specificity, both parameters are optimized resulting in substantial gains in accuracy which are clearly reflected in the data.”
In this complementary role, AI can achieve numerous objectives in clinical workflows:
Beyond flagging various pathologies, AI-centered care coordination tools have worked with great success. This means that once a suspected pathology is flagged, designated specialists and broader care teams are brought into the fold with immediate access to EMRs, relevant images and a chat tool. The direct result is streamlined care for patients in critical need and thus, improved patient outcomes. As said by Dr. Dana Tomalty, Interventional Radiologist at Huntsville Hospital, AI-driven care coordination has “decreased the length of latency time from the time the patient hits the CT scan until they are in the angio suite by a huge amount.”
The Adoption of Healthcare AI
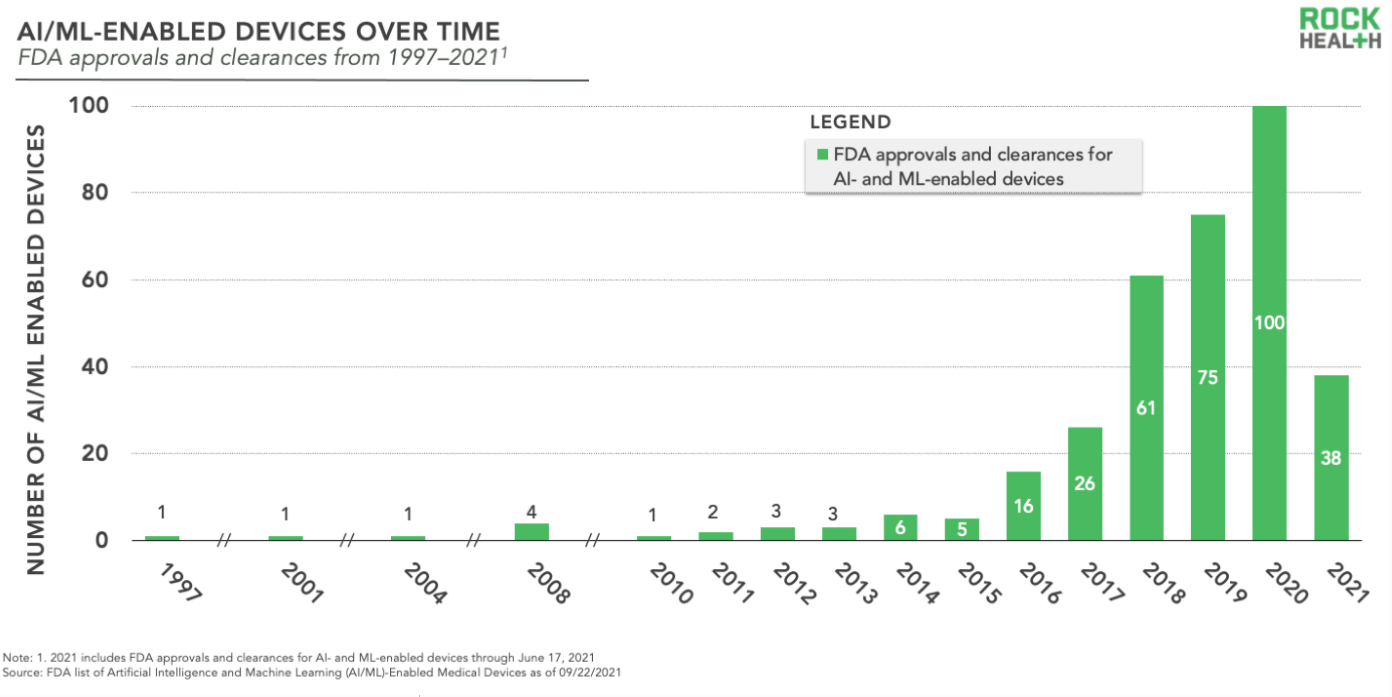
One could cite 2018 as the year where AI solutions went from secondary to mainstream. This was the first year in which over 50 AI-based healthcare products received FDA clearance. Those numbers have grown exponentially since then, as indicated in the graph below:
At Aidoc alone, our AI is currently analyzing over 2 million patients a year. With other strong companies such as RapidAI, Viz.ai, Bayesian Health, Heartflow and Cleerly, I believe that up to 30% of patient care is already benefiting from the utilization of clinical AI solutions.
Consider this: just three years ago, that 30% figure was less than 1%, making AI one of the fastest adopted technologies in healthcare.
Overcoming the Challenges of AI
While the success and progress of AI are undeniable, we’re still faced with some noteworthy challenges of AI in healthcare moving forward. According to a 2021 report from Optum, “an overwhelming 98% of health care leaders say their organization either has or is planning to implement an AI strategy.” The problem comes not in the openness to adopting AI (or lack thereof) into hospital and healthcare workflows, but, as the Politico writers note, it lies in infrastructure and the fact that “every health system is unique in its technology and the way it treats patients. That means an algorithm may not work as well everywhere.”
That is absolutely right. There are tons of great AI vendors out there providing a variety of FDA-cleared algorithms. However, a common criticism is that some algorithms on the market perform very well in internal testing, but externally (or “in the wild” as we like to call it) they prove less effective because they may have not been tested on an adequately robust and diverse dataset. Every hospital serves different demographics and has its own unique infrastructure and dataset, and AI must be effectively deployed within these circumstances.
Another problem is collating and orchestrating the data. Because hospital administrators want to integrate AI into their hospital workflows, how can numerous algorithms (potentially from different vendors) work together so as not to interfere with the physicians’ workflow and without disrupting one another on the backend? This is where orchestration comes into play.
Therefore, we believe in the concept of the Artificial Intelligence Operating System (aiOS). An algorithm doesn’t exist in a vacuum, but in relation to other algorithms, which necessitates an aiOS to serve as an orchestrator that can:
a. Help the partner acquire deidentified data to sustain high algorithmic integrity and
b. Make sure that data and algorithms within a health system are effectively collating data and giving end users actionable insights.
Healthcare AI is still in its early stages, and with an estimated $67.4 billion worth of investment in by 2027, the hype is real. Investors are confident in the potential for AI to become a key player in the future of medicine. At Aidoc, we’re proud to say that our healthcare AI has already shown that its implementation results in real improved patient outcomes. The market needs healthcare AI to continue evolving and playing a central role in improving hospital workflows, care coordination and eventually, an end-to-end solution to address multiple points on the patient care continuum.